1 材料与方法
1.1 样品采集
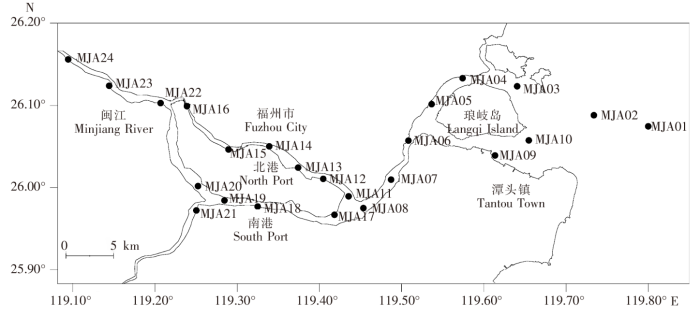
图1
1.2 仪器与试剂
液相色谱质谱联用仪(HPLC-MS/MS)(Agilent 6490,美国Agilent);醋酸纤维膜(0.45 μm,天津津腾实验设备有限公司);大体积采样器(匹配20 mL SPE柱,美国Supelco);固相萃取装置(12通道,德国CNW);真空泵(GM-0.33型,天津津腾实验设备有限公司);Oasis HLB柱(1 g/20 mL,美国Waters);PTFE针筒式滤膜(13 mm×0.22 μm,天津贺世科技发展有限公司)。甲酸、乙腈和甲醇均为色谱纯级,其中乙腈和甲醇购自美国Tedia公司,甲酸购自上海Aladdin试剂有限公司;超纯水取自Milli-Q Advantage纯水机(美国Millipore);乙二胺四乙酸二钠(Na2EDTA,分析纯,上海申博化工有限公司)、二氯甲烷(色谱纯,美国Tedia)。
88种抗生素包括23种磺胺类(Sulfonamides,SAs)、17种喹诺酮类(Quinolones,QNs)、9种大环内酯类(Macrolides,MLs)、8种四环素类(Tetracyclines,TCs)、12种β-内酰胺类(β-Lactams,β-Ls)、8种硝基呋喃及其代谢物类(Nitrofurans and metabolites derivatives of nitrofurans,NFs and NPs)、5种非类固醇类(Non-steroidal anti-inflammatory drugs,NSAIDs)、3种氯霉素类(Chloramphenicols,CAPs)、3种硝基咪唑类(Nitroimidazoles,NIZs)。13种替代物包括磺胺噻唑-13C6(Sulfathiazole-13C6,STZ-13C6)、磺胺喹恶啉-13C6(Sulfaquinoxaline-13C6,SQ-13C6)、磺胺二甲氧嘧啶-D6(Sulfadimethoxine-D6,SDM-D6)、磺胺嘧啶-D4(Sulfadiazine-D4,SDZ-D4)、甲氧苄啶-13C3(Trimethoprim-13C3,TMP-13C3)、NP-AOZ-D4、NP-AMOZ-D5、NP-AHD-13C3、氯霉素-D5(Chloramphenicol-D5,CAP-D5)、环丙沙星-D8(Ciprofloxacin-D8,CIP-D8)、诺氟沙星-D4(Norfloxacin-D4,NOR-D4)、恩诺沙星-D5(Enrofloxacin-D5,EF-D5)、噻苯咪唑-D6(Thiabendazole-D6,TBZ-D6)。1种内标物为磺胺噻唑-D4(Sulfathiazole-D4,SAZ-D4)。其中,环丙沙星(Ciprofloxacin,CIP)、诺氟沙星(Norfloxacin,NOR)、恩诺沙星(Enrofloxacin,EF)、氧氟沙星(Ofloxacin,OF)、达氟沙星(Danofloxacin,DAN)、氟甲喹(Flumequine,FQ)、麻保沙星(Marbofloxacin,MB)、沙拉沙星(Sarafloxacin,SR)、恶喹酸(Oxolinic acid,QA)和CAP-D5均购自美国Sigma-Alorich公司;CIP-D8和EF-D5均购自上海安谱实验科技股份有限公司;SAZ-D4、TMP-13C3、STZ-13C6和SDZ-D4均购自加拿大 Toronto Research chemicals 公司;SQ-13C6、NOR-D4、NP-AOZ-D4、NP-AMOZ-D5 和 NP-AHD-13C3 均购自德国WITEGA 公司;其他标准品均购自德国Dr.Ehrenstorfer GmbH 公司。
88种抗生素混合标准溶液配制:分别称取一定质量的目标抗生素标准品,其中四环素、金霉素、土霉素与尼卡巴嗪溶解于纯水中,β-内酰胺类药品溶解于乙腈-水(1∶1,V/V)中,其他药品则分别溶解于甲醇中,配制成200.0 mg/L单标储备液,并于-18°C冰箱中保存。以 含0.1%甲酸(V/V)的甲醇-水(2∶8,V/V)为溶剂将上述抗生素单标储备液分组配制成实验所需浓度的混合标准工作液。
13种同位素标记物混合标准溶液的配制:分别称取一定质量的同位素标准品,以甲醇为定容溶剂,配置成100 mg/L单标储备液,并于-18°C冰箱中保存。以含0.1%甲酸(V/V)的甲醇-水(2∶8,V/V)为溶剂将上述同位素标准品的单标储备液配制成实验所需浓度的替代物混合标准工作液。
1种内标物混合标准溶液的配制:磺胺噻唑-D4的单标储备液配制与13种同位素标记物相同,最后以含0.1%甲酸(V/V)的甲醇-水(2∶8,V/V)为溶剂将磺胺噻唑-D4配制成实验所需浓度的内标物混合标准工作液。
各目标抗生素的名称和分组编号列于附表1。
附表1 目标抗生素、替代物和内标物的 HPLC-MS/MS 测定的相关参数
Appendix.1
| 编号 Number | 名称 Name | 保留 时间/min Retention time | MRM扫描模式相关参数 MRM parameters | 线性范围/ (μg/L) Linear range | 线性相 关系数R2 Linear correlation coefficient | 仪器 检出限/ (μg/L) Instrument detection limits | 方法检 出限/ (ng/L) Method detection limits | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 离子源 模式 Ion source mode | 母离子 Parent ion | 子离子 Daughter ion | 碰撞能/eV Collision energy | ||||||||||||
| Su | 替代物Surrogates | ||||||||||||||
| Su1 | 磺胺噻唑-13C6 Sulfathiazole-13C6 | 10.577 | ESI+ | 262.0 | 162.0*/114.0 | 10/20 | 0.5~100 | 0.997 7 | 0.10 | 0.10 | |||||
| Su2 | 磺胺喹恶啉-13C6 Sulfaquinoxaline-13C6 | 25.649 | ESI+ | 307.1 | 162.0*/114.0 | 10/15 | 1.0~100 | 0.999 4 | 0.10 | 0.10 | |||||
| Su3 | 磺胺二甲氧嘧啶-D6 Sulfadimethoxine-D6 | 25.449 | ESI+ | 317.1 | 162.2*/251.1/223.9 | 15/15/25 | 0.1~100 | 0.998 6 | 0.02 | 0.02 | |||||
| Su4 | 磺胺嘧啶-D4 Sulfadiazine-D4 | 8.673 | ESI+ | 255.1 | 160.1*/112.1 | 10/25 | 0.1~100 | 0.998 6 | 0.01 | 0.01 | |||||
| Su5 | 甲氧苄啶-13C3 Trimethoprim-13C3 | 9.865 | ESI+ | 294.2 | 231.0*/277.1/262.2 | 18/20/20 | 0.1~100 | 0.997 7 | 0.001 | 0.001 | |||||
| Su6 | NP-AOZ-D4 | 24.240 | ESI+ | 239.8 | 166.4* | 5 | 5.0~100 | 0.999 7 | 0.05 | 0.05 | |||||
| Su7 | NP-AMOZ-D5 | 11.600 | ESI+ | 340.1 | 296.2*/265.1/133.0 | 5/10/20 | 5.0~100 | 0.999 1 | 0.05 | 0.05 | |||||
| Su8 | NP-AHD-13C3 | 21.803 | ESI+ | 252.0 | 176.2*/134.2 | 20/30 | 5.0~500 | 0.999 6 | 0.10 | 0.10 | |||||
| Su9 | 氯霉素-D5 Chloramphenicol-D5 | 4.959 | ESI- | 328.2 | 157.0*/126.0 | 10、/2 | 0.5~100 | 0.999 9 | 0.01 | 0.01 | |||||
| Su10 | 环丙沙星-D8 Ciprofloxacin-D8 | 13.100 | ESI+ | 340.2 | 296.2*/249.1 | 15/26 | 0.5~100 | 0.998 5 | 0.10 | 0.10 | |||||
| Su11 | 诺氟沙星-D4 Norfloxacin-D4 | 12.408 | ESI+ | 325.2 | 307.1*/281.2/238.1 | 20/15/20 | 0.5~100 | 0.996 6 | 0.04 | 0.04 | |||||
| Su12 | 恩诺沙星-D5 Enrofloxacin-D5 | 15.858 | ESI+ | 365.2 | 321.2*/245.1 | 20/30 | 0.5~100 | 0.999 6 | 0.04 | 0.04 | |||||
| Su13 | 噻苯咪唑-D6 Thiabendazole-D6 | 9.386 | ESI+ | 208.1 | 180.1*/181.1/135.8 | 15/25/30 | 0.1~100 | 0.999 2 | 0.005 | 0.005 | |||||
| Is | 内标物Internalstandard | ||||||||||||||
| Is1 | 磺胺噻唑-D4 Sulfathiazole-D4 | 10.200 | ESI+ | 260.0 | 159.9*/112.0 | 5/20 | 0.5~100 | 0.999 9 | 0.10 | 0.10 | |||||
| S | 磺胺类Sulfonamides | ||||||||||||||
| S01 | 磺胺甲恶唑 Sulfamethoxazole | 21.700 | ESI+ | 254.1 | 156.1*/160.1 | 10/15 | 0.5~100 | 0.999 3 | 0.01 | 0.01 | |||||
| S02 | 磺胺甲噻二唑 Sulfamethizole | 16.332 | ESI+ | 271.0 | 156.0*/108.1 | 10/20 | 0.1~100 | 0.999 4 | 0.02 | 0.02 | |||||
| S03 | 磺胺吡啶 Sulfapyridine | 10.711 | ESI+ | 250.0 | 156.0*/184.1 | 10/15 | 0.5~100 | 0.999 4 | 0.05 | 0.05 | |||||
| S04 | 磺胺噻唑 Sulfathiazole | 10.599 | ESI+ | 256.0 | 156.0*/108.0 | 10/20 | 0.5~100 | 0.999 4 | 0.10 | 0.10 | |||||
| S05 | 磺胺喹恶啉 Sulfaquinoxaline | 25.672 | ESI+ | 301.0 | 156.0*/208.0 | 10/15 | 0.5~100 | 0.998 0 | 0.10 | 0.10 | |||||
| S06 | 磺胺氯哒嗪 Sulfachloropyridazine | 19.895 | ESI+ | 285.0 | 156.0*/108.0 | 10/20 | 0.1~100 | 0.999 0 | 0.02 | 0.02 | |||||
| S07 | 磺胺甲基嘧啶 Sulfamerazine | 11.750 | ESI+ | 265.1 | 172.0*/156.0 | 10/10 | 0.5~100 | 0.999 6 | 0.02 | 0.02 | |||||
| S08 | 磺胺二甲氧嘧啶 Sulfadimethoxine | 20.645 | ESI+ | 311.1 | 156.0*/245.1/218.0 | 18/15/15 | 0.1~100 | 0.999 5 | 0.02 | 0.02 | |||||
| S09 | 磺胺对甲氧嘧啶 Sulfamethoxydiazine | 16.331 | ESI+ | 281.1 | 156.0*/188.0 | 10/10 | 0.1~20 | 0.999 9 | 0.05 | 0.05 | |||||
| S10 | 磺胺间甲氧嘧啶 Sulfamonomethoxine | 16.331 | ESI+ | 281.0 | 156.0*/215.1 | 15/15 | 0.1~100 | 0.999 9 | 0.01 | 0.01 | |||||
| S11 | 磺胺二甲基嘧啶 Sulfamethazine | 14.427 | ESI+ | 279.1 | 156.0/186.0* | 15/15 | 0.5~100 | 0.999 3 | 0.01 | 0.01 | |||||
| S12 | 磺胺嘧啶 Sulfadiazine | 8.785 | ESI+ | 251.0 | 156.0*/185.1 | 10/15 | 1.0~100 | 0.999 5 | 0.01 | 0.01 | |||||
| S13 | 磺胺二甲基异嘧啶 Sulfaisodimidine | 14.427 | ESI+ | 279.0 | 124.1*/186.0/108.0 | 20/10 | 0.5~100 | 0.999 1 | 0.02 | 0.02 | |||||
| S14 | 磺胺醋酰 Sulfacetamide | 7.614 | ESI+ | 215.0 | 156.0*/108.0 | 5/15 | 0.5~50 | 0.996 2 | 0.50 | 0.50 | |||||
| S15 | 磺胺二甲异恶唑 Sulfisoxazole | 23.400 | ESI+ | 268.0 | 156.0*/113.0 | 10/10 | 0.1~100 | 0.999 4 | 0.01 | 0.01 | |||||
| S16 | 磺胺硝苯 Sulfanitran | 29.056 | ESI+ | 336.0 | 156.1*/294.0 | 5/5 | 0.5~500 | 0.999 0 | 0.10 | 0.10 | |||||
| S17 | 磺胺甲氧哒嗪 Sulfamethoxypyridazine | 19.200 | ESI+ | 281.0 | 156.0*/126.0/108.0 | 10/15/20 | 0.5~100 | 0.999 4 | 0.04 | 0.04 | |||||
| S18 | 磺胺胍 Sulfaguanidine | 7.614 | ESI+ | 215.1 | 156.1*/108.1 | 15/20 | 5.0~100 | 0.998 2 | 1.00 | 1.00 | |||||
| S19 | 甲氧苄啶 Trimethoprim | 9.865 | ESI+ | 291.2 | 230.1*/261.0 | 20/25 | 0.1~100 | 0.999 7 | 0.001 | 0.001 | |||||
| S20 | 磺胺二甲恶唑 Sulfamoxol | 13.631 | ESI+ | 268.0 | 156.0*113.0 | 15/15 | 0.1~100 | 0.999 4 | 0.02 | 0.02 | |||||
| S21 | 磺胺苯吡唑 Sulfaphenazole | 26.003 | ESI+ | 315.1 | 156.0*/221.9 | 15/20 | 0.1~100 | 0.998 8 | 0.01 | 0.01 | |||||
| S22 | 磺胺邻二甲氧嘧啶 Sulfadoxine | 20.645 | ESI+ | 311.1 | 156.1*/108.1 | 25/30 | 0.1~100 | 0.999 9 | 0.01 | 0.01 | |||||
| S23 | 磺胺苯酰 Sulfabenzamide | 25.165 | ESI+ | 277.1 | 108.0*/156.0 | 25/20 | 0.1~100 | 0.999 9 | 0.01 | 0.01 | |||||
| Q | 喹诺酮类Quinolones | ||||||||||||||
| Q01 | 环丙沙星 Ciprofloxacin | 13.227 | ESI+ | 332.1 | 314.1*/288.1 | 15/15 | 0.5~100 | 0.999 8 | 0.10 | 0.10 | |||||
| Q02 | 诺氟沙星 Norfloxacin | 12.497 | ESI+ | 320.1 | 302.1*/276.1 | 15/10 | 0.5~100 | 0.999 4 | 0.10 | 0.10 | |||||
| Q03 | 恩诺沙星 Enrofloxacin | 15.903 | ESI+ | 360.1 | 342.1*/316.1 | 15/15 | 0.5~100 | 0.999 6 | 2.00 | 2.00 | |||||
| Q04 | 氧氟沙星 Ofloxacin | 12.405 | ESI+ | 362.1 | 318.1*/261.0 | 15/20 | 0.5-100 | 0.999 7 | 0.04 | 0.04 | |||||
| Q05 | 达氟沙星 Danofloxacin | 14.974 | ESI+ | 358.1 | 340.0*/283.1 | 20/20 | 5.0~100 | 0.999 8 | 0.10 | 0.10 | |||||
| Q06 | 氟甲喹 Flumequine | 27.912 | ESI+ | 262.0 | 244.0*/202.0 | 15/20 | 0.1~50 | 0.997 6 | 0.02 | 0.02 | |||||
| Q07 | 麻保沙星 Marbofloxacin | 10.877 | ESI+ | 363.1 | 345.1*/320.0 | 15/20 | 1.0~500 | 0.997 8 | 0.50 | 0.50 | |||||
| Q08 | 沙拉沙星 Sarafloxacin | 18.115 | ESI+ | 386.0 | 368.0*/342.1/299.0 | 20/15/25 | 1.0~100 | 0.999 6 | 0.10 | 0.10 | |||||
| Q09 | 恶喹酸 Oxolinic acid | 28.300 | ESI+ | 262.0 | 244.0*/216.0 | 12 | 0.5~100 | 0.997 6 | 0.04 | 0.04 | |||||
| Q10 | 洛美沙星 Lomefloxacin | 14.110 | ESI+ | 352.2 | 308.1*/264.9 | 10/20 | 0.5~100 | 0.997 8 | 0.05 | 0.05 | |||||
| Q11 | 萘啶酸 Nalidixic acid | 27.030 | ESI+ | 233.1 | 215.0*/187.0 | 15/20 | 0.1~100 | 0.998 0 | 0.05 | 0.05 | |||||
| Q12 | 双氟沙星 Difloxacin | 18.491 | ESI+ | 400.2 | 382.1*/356.0 | 20/10 | 0.5~100 | 0.999 6 | 0.10 | 0.10 | |||||
| Q13 | 奥比沙星 Orbifloxacin | 16.078 | ESI+ | 396.2 | 352.1*/295.0 | 15/25 | 0.5~50 | 0.998 4 | 0.04 | 0.04 | |||||
| Q14 | 氟罗沙星 Fleroxacin | 12.271 | ESI+ | 370.0 | 326.0*269.0 | 20/25 | 0.5~100 | 0.999 6 | 0.10 | 0.10 | |||||
| Q15 | 依诺沙星 Enoxacin | 11.301 | ESI+ | 321.4 | 303.3*/233.9 | 20/20 | 5.0~100 | 0.999 6 | 1.00 | 1.00 | |||||
| Q16 | 司帕沙星 Sparfloxacin | 18.536 | ESI+ | 393.0 | 292.0*/349.0 | 25/20 | 1.0~100 | 0.998 4 | 0.10 | 0.10 | |||||
| Q17 | 培氟沙星 Pefloxacin | 13.000 | ESI+ | 334.3 | 290.3*/233.2 | 15/25 | 0.1~100 | 0.999 8 | 0.04 | 0.04 | |||||
| M | 大环内酯类Macrolides | ||||||||||||||
| M01 | 红霉素 Erythromycin | 24.842 | ESI+ | 734.4 | 576.4*/158.1 | 15/20 | 1.0~100 | 0.999 2 | 0.20 | 0.20 | |||||
| M02 | 泰乐菌素 Tylosin | 25.372 | ESI+ | 916.4 | 772.3/174.1* | 30/40 | 5.0~100 | 0.999 7 | 0.40 | 0.40 | |||||
| M03 | 替米考星 Tilmicosin | 22.428 | ESI+ | 869.5 | 696.3/174.1* | 40/45 | 1.0~100 | 0.999 5 | 0.01 | 0.01 | |||||
| M04 | 林可霉素 Lincomycin | 6.491 | ESI+ | 407.2 | 359.1/126.1* | 15/20 | 1.0~100 | 0.999 2 | 0.01 | 0.01 | |||||
| M05 | 交沙霉素 Josamycin | 28.400 | ESI+ | 828.3 | 109.0*/174.0 | 15/15 | 1.0~100 | 0.995 8 | 1.00 | 1.00 | |||||
| M06 | 螺旋霉素 Spiramycin | 25.400 | ESI+ | 875.4 | 174.3*/145.3 | 35/35 | 10.0~1 000 | 0.997 7 | 4.00 | 4.00 | |||||
| M07 | 白霉素 Kitasamycin | 26.303 | ESI+ | 772.4 | 174.4*/109.1 | 35/35 | 1.0~100 | 0.999 9 | 0.20 | 0.20 | |||||
| M08 | 泰拉菌素 Tulathromycin | 15.170 | ESI+ | 404.0 | 158.1*/72.0 | 20/20 | 1.0~100 | 0.999 4 | 0.10 | 0.10 | |||||
| M09 | 延胡索酸泰妙菌素 Tiamulinfumarate | 26.437 | ESI+ | 494.3 | 192.1*/119.0 | 15/30 | 0.5~100 | 0.999 8 | 0.01 | 0.01 | |||||
| T | 四环素类Tetracylcines | ||||||||||||||
| T01 | 土霉素 Oxytetracycline | 12.002 | ESI+ | 461.1 | 443.1/426.1* | 5/15 | 1.0~500 | 0.999 5 | 0.20 | 0.20 | |||||
| T02 | 金霉素 Chlortetracycline | 19.900 | ESI+ | 479.1 | 462.1/444.1* | 10/15 | 5.0~500 | 0.999 2 | 0.50 | 0.50 | |||||
| T03 | 四环素 Tetracycline | 13.800 | ESI+ | 445.1 | 427.1/410.0* | 515 | 5.0~500 | 0.998 4 | 0.50 | 0.50 | |||||
| T04 | 强力霉素 Doxycycline | 10.800 | ESI+ | 445.1 | 428.1*/410.1 | 15/20 | 5.0~500 | 0.999 0 | 0.50 | 0.50 | |||||
| T05 | 去甲基金霉素 Demeclocycline | 17.382 | ESI+ | 465.2 | 448.0*/430.0 | 15/20 | 5.0~500 | 0.996 8 | 5.00 | 5.00 | |||||
| T06 | 脱水四环素 Anhydrotetracycline | 24.888 | ESI+ | 427.0 | 154.0*/410.0 | 20/35 | 5.0~500 | 0.996 0 | 5.00 | 5.00 | |||||
| T07 | 二甲胺四环素 Minocycline | 11.000 | ESI+ | 458.2 | 441.2*/351.9 | 20/40 | 5.0~500 | 0.998 3 | 0.50 | 0.50 | |||||
| T08 | 美他环素 Methacycline | 20.349 | ESI+ | 443.1 | 426.1*/381.2 | 20/25 | 5.0~500 | 0.999 0 | 0.40 | 0.40 | |||||
| bL | β-内酰胺类β-lactams | ||||||||||||||
| bL01 | 阿莫西林 Amoxicillin | 8.108 | ESI+ | 398.1 | 349.1*/160.0 | 10/20 | 5.0~100 | 0.999 9 | 0.50 | 0.50 | |||||
| bL02 | 头孢噻呋 Ceftiofur | 12.500 | ESI+ | 524.0 | 241.0*/285.0 | 10/15 | 0.5~100 | 0.999 9 | 0.20 | 0.20 | |||||
| bL03 | 青霉素 G Penicillin G | 10.902 | ESI+ | 335.1 | 160.1*/176.1 | 20/15 | 0.5~100 | 0.999 8 | 0.05 | 0.05 | |||||
| bL04 | 双氯青霉素 Dicloxacillin | 32.857 | ESI+ | 502.0 | 160.1/212.1* | 15/20 | 0.5~100 | 0.998 4 | 0.20 | 0.20 | |||||
| bL05 | 苯唑青霉素 Oxacillin | 29.273 | ESI+ | 402.1 | 160.0/242.9* | 30/15 | 0.5~100 | 0.999 1 | 0.20 | 0.20 | |||||
| bL06 | 氯唑青霉素 Cloxacillin | 31.154 | ESI+ | 436.1 | 160.2/277.2* | 15/20 | 0.1~20 | 0.999 3 | 0.05 | 0.05 | |||||
| bL07 | 氨苄青霉素 Ampicillin | 7.601 | ESI+ | 350.1 | 160.0/106.1* | 10/15 | 1.0~100 | 0.999 9 | 0.40 | 0.40 | |||||
| bL08 | 青霉素 V Penicillin V | 27.881 | ESI+ | 351.1 | 160.0*/113.9 | 10/35 | 1.0~100 | 0.997 1 | 1.00 | 1.00 | |||||
| bL09 | 萘夫西林 Nafcillin | 31.529 | ESI+ | 469.1 | 391.1*/310.0 | 15/15 | 1.0~100 | 0.998 5 | 0.40 | 0.40 | |||||
| bL10 | 哌拉西林 Piperacillin | 25.573 | ESI+ | 518.2 | 159.8/143.0* | 30/30 | 5.0~200 | 0.999 4 | 1.00 | 1.00 | |||||
| bL11 | 头孢匹林 Cefapirn | 4.763 | ESI+ | 424.0 | 292.0*/181.0/151.9 | 10/20/20 | 10.0~500 | 0.999 6 | 0.40 | 0.40 | |||||
| bL12 | 头孢氨苄 Cephalexin | 12.605 | ESI+ | 348.0 | 158.0*/140.0 | 10/15 | 10.0~500 | 0.999 3 | 1.00 | 1.00 | |||||
| N | 硝基呋喃及其代谢物类Nitrofuransandmetabolitesderivativesofnitrofurans | ||||||||||||||
| N01 | 呋喃唑酮 Furazolidone | 17.355 | ESI+ | 226.1 | 122.1*/138.7 | 20/10 | 5.0~500 | 0.998 8 | 0.05 | 0.05 | |||||
| N02 | 呋喃它酮 Furaltadone | 7.161 | ESI+ | 325.1 | 252.1*/281.1 | 10/5 | 5.0~100 | 0.999 3 | 0.10 | 0.10 | |||||
| N03 | 呋喃妥因 Nitrofurantoin | 15.200 | ESI+ | 239.0 | 222.0*/122.0 | 10/20 | 5.0~500 | 0.999 6 | 0.10 | 0.10 | |||||
| N04 | 呋喃西林 Nitrofurazone | 12.973 | ESI+ | 199.1 | 182.0*/139.1/136.1 | 5/5/10 | 5.0~500 | 0.998 2 | 0.10 | 0.10 | |||||
| N05 | NP-AOZ | 24.395 | ESI+ | 236.0 | 134.0*/104.0 | 5/20 | 5.0~100 | 0.996 3 | 0.05 | 0.05 | |||||
| N06 | NP-AMOZ | 11.898 | ESI+ | 335.1 | 291.1*/262.1 | 5/10 | 5.0~100 | 0.997 5 | 0.05 | 0.05 | |||||
| N07 | NP-AHD | 20.608 | ESI+ | 249.0 | 134.0*/178.1 | 5/10 | 5.0~500 | 0.999 6 | 0.10 | 0.10 | |||||
| N08 | NP-SCA | 21.164 | ESI+ | 209.0 | 192.0*/166.0 | 5/5 | 2.5~500 | 0.999 6 | 0.10 | 0.10 | |||||
| NAD | 非类固醇类Non-steroidalanti-inflammatorydrugs | ||||||||||||||
| NAD01 | 萘普生 Naproxen | 32.166 | ESI+ | 231.0 | 185.1*/170.0 | 5/20 | 0.5~100 | 0.999 6 | 1.00 | 1.00 | |||||
| NAD02 | 酮洛芬 Ketoprofen | 31.987 | ESI+ | 255.1 | 105.0*/209.0 | 20/10 | 0.1~100 | 0.999 1 | 0.05 | 0.05 | |||||
| NAD03 | 布洛芬 Ibuprofen | 11.186 | ESI- | 204.9 | 161.0* | 5 | 0.5~100 | 0.999 2 | 0.20 | 0.20 | |||||
| NAD04 | 托芬那酸 TolfenamicAcid | 12.594 | ESI- | 259.9 | 216.0*/214.0 | 20/20 | 0.5~100 | 0.997 9 | 0.40 | 0.40 | |||||
| NAD05 | 安乃近 Analgin | 4.678 | ESI+ | 218.1 | 97.0/56.0* | 15/10 | 0.1~100 | 0.998 5 | 0.04 | 0.04 | |||||
| C | 氯霉素类Chloramphenicols | ||||||||||||||
| C01 | 氯霉素 Chloramphenicol | 4.980 | ESI- | 321.1 | 257.0/151.0* | 5/10 | 0.5~100 | 0.999 9 | 0.01 | 0.01 | |||||
| C02 | 甲砜霉素 Thiamphenicol | 4.113 | ESI- | 354.1 | 290.0/185.1* | 5/15 | 0.5~500 | 0.999 9 | 0.01 | 0.01 | |||||
| C03 | 氟甲砜霉素 Florfenicol | 5.026 | ESI- | 356.1 | 336.2/185.0* | 10/12 | 0.5~500 | 0.998 9 | 0.01 | 0.01 | |||||
| NZNi | 硝基咪唑类 Troimidazoles | ||||||||||||||
| NZ01 | 甲硝唑 Metronidazole | 6.508 | ESI+ | 172.0 | 128.2/82.1* | 21/35 | 0.5~100 | 0.999 9 | 0.04 | 0.04 | |||||
| NZ02 | 二甲硝咪唑 Dimetridazole | 9.033 | ESI+ | 142.0 | 96.0*/81.0 | 23/36 | 0.5~100 | 0.999 9 | 0.05 | 0.05 | |||||
| NZ03 | 洛硝达唑 Ronidazole | 7.991 | ESI+ | 201.1 | 140.2*/110.2 | 17/25 | 1.0~100 | 0.999 8 | 0.40 | 0.40 | |||||
注:带“*”号标识的为定量离子
Note:*identified as quantitative ions.
1.3 预处理与测定
预处理方法及仪器分析方法,参照庄姗姗[15]的研究。量取1 L水样经0.45 μm滤膜过滤后,加入0.5 g Na2EDTA,并加入替代物,混匀,以4~6 mL/min流速通过已活化HLB柱(依次用20 mL甲醇和6 mL超纯水活化);上柱完毕后以10 mL甲醇-水(5∶95,V/V)淋洗,随后抽干并依次用8 mL甲醇、8 mL含0.1%甲酸(V/V)的甲醇和6 mL甲醇-二氯甲烷(1∶1,V/V)洗脱;接取洗脱液,置于40℃下氮吹浓缩至干,加入一定量的内标物,用含0.1%甲酸(V/V)的甲醇-水(2∶8,V/V)定容至1.0 mL,经0.22 μm PTFE针头式过滤器过滤至进样小瓶中,待HPLC-MS/MS检测。
质谱参数:电喷雾离子源(Electron spray ionization,ESI),检测模式为多反应离子选择监测(Multiple reaction monitoring,MRM);鞘气温度及流速分别设定为350℃和12 L/min;干燥气温度及流速分别设定为300℃和10 L/min,鞘气和干燥气均由氮气发生器提供;雾化气压力(Nebulizer pressure)定为241.32 kPa;喷嘴电压和毛细管电压分别设为 1 500 V 和4 000 V;碰撞气使用的是高纯氮气(99.999%);碎裂电压为380 V。目标物母离子和子离子以及碰撞能等相关信息见附表1。
液相色谱参数:色谱柱为Phenomenex Kinetex C18柱(2.6 μm×150 mm×3 mm i.d.,Phenomenex,USA);流动相流速:0.25 mL/min;进样量:10.0 μL;88种目标物分为ESI+项目和ESI-项目两组。ESI+项目组的流动相为超纯水(A)和含0.1%甲酸(V/V)的乙腈(B1),梯度洗脱程序为0 ~2.00 min,B1为10%;2.00~10.00 min,B1从10%升至15%,10.00~12.00 min,B1 15%保持;12.00~14.00 min,B1从15%升至20%,14.00~16.00 min,B1 20%保持;16.01~20.00 min,B1从20%升至25%;20.00~23.00 min,B1从25%升至40%;23.00~27.00 min,B1 40%保持;27.00~34.00 min,B1从40%升至80%;34.00~41.00 min,B1从80%升至90%;41.01~46.00 min,B1为10%。ESI-项目组的流动相为超纯水(A)和乙腈(B2),梯度洗脱程序为0~1.00 min,B2为25%;1.01~5.00 min,B2为45%;5.00~9.00 min,B2从45%升至80%;9.00~12.00 min,B2 80%保持;12.01~16.00 min,B2为25%。
1.4 风险评价
式(1)~(2)中,MEC为抗生素测定含量,ng/L;PNEC为预计无效应浓度,ng/L;LC50 为半数致死浓度,ng/L;EC50 为半数效应浓度,ng/L;AF 为标准评价因子,对于急性毒性数据和慢性毒性数据分别取1 000和100。
式(3)中,i为第i种抗生素,i=1,2,…,n;ECxalgae:以藻类为测试生物的效应浓度,ng/L;ECxdaphnids:以蚤类为测试生物的效应浓度,ng/L;ECxfish:以鱼类为测试生物的效应浓度。风险评价相关参数见附表2。通常将生态风险程度划分为3个级别:当RQ或MHQ<0.1时,表示低生态风险;当0.1≤RQ或MHQ<1.0时,表示中等生态风险;当RQ或MHQ≥1.0时,表示高生态风险。
附表2 各抗生素生态风险评价相关参数
Appendix.2
| 名称 Name | 最敏感物种 The most sensitive species | 毒性类型 Toxicity type | AF | EC50/(mg/L) | PNEC/(ng/L) |
|---|---|---|---|---|---|
| 磺胺甲恶 Sulfamethoxazole | 聚球藻(S.leopoliensis) | 急性毒性 | 1 000 | 0.027 | 27 |
| 磺胺吡啶 Sulfapyridine | 小球藻(Chlorella) | 急性毒性 | 1 000 | 5.28 | 5 280 |
| 磺胺氯哒嗪Sulfamonomethoxine | 小球藻(Chlorella) | 急性毒性 | 1 000 | 32.25 | 32 250 |
| 磺胺二甲基嘧啶 Sulfamethazine | 栅列藻(S.vacuolatus) | 急性毒性 | 1 000 | 19.52 | 19 520 |
| 磺胺嘧啶 Sulfadiazine | 铜绿微囊藻(M.aeruginosa) | 急性毒性 | 1 000 | 0.135 | 135 |
| 磺胺邻二甲氧嘧啶 Sulfadoxine | 小球藻(Chlorella) | 急性毒性 | 1 000 | 3.82 | 3 820 |
| 甲氧苄啶 Trimethoprim | 有孔虫(Rsalina) | 急性毒性 | 1 000 | 16 | 16 000 |
| 红霉素 Erythromycin | 近头状伪蹄形藻(P.subcapitata) | 急性毒性 | 1 000 | 0.02 | 20 |
| 林可霉素 Lincomycin | 近头状伪蹄形藻(P.subcapitata) | 急性毒性 | 1 000 | 0.05 | 50 |
| 氟甲砜霉素 Florfenicol | 羊角月牙藻(S.capricornutum) | 急性毒性 | 1 000 | 8.886 | 8 886 |
| 甲砜霉素 Thiamphenicol | 铜绿微囊藻(M.aeruginosa) | 急性毒性 | 1 000 | 0.32 | 320 |
| 甲硝唑 Metronidazole | 小球藻(Chlorella) | 急性毒性 | 1 000 | 1.25 | 12 500 |
1.5 数据质控
采用内标法定量,并通过全程空白、基底加标实验、同位素替代物以及基质效应评估等进行质量控制。样品测定过程中,空白样品均未检出目标抗生素;旱季和雨季批次各进行了一次样品的基底加标回收实验,在20 ng/L(n=3)和100 ng/L(n=3)加标浓度下,回收率在40%~130%之间且RSD≤30%的目标抗生素分别占总数的95.6%和97.0%;13种同位素替代物中,除氘代氯霉素的回收率略微偏低(在30%~40%之间,基质效应校正后可在80%~100%)外,其余12种同位素的回收率均在40%~130%之间。综上,认为样品分析过程的质量控制合格,结果准确可靠。两批次样品替代物回收率详情见附表3。
附表3 旱季与雨季两批次样品替代物回收率
Appendix.3
| 替代物名称 Name of surrogates | 旱季批次(n=24) Batch of dry season(n=24) | 雨季批次(n=24) Batch of rainy season(n=24) |
|---|---|---|
| 平均回收率±标准偏差/% Average recovery±standard deviations | ||
| 磺胺噻唑-13C6 Sulfathiazole-13C6 | 83.7±6.4 | 90.8±7.9 |
| 磺胺喹恶啉-13C6 Sulfaquinoxaline-13C6 | 49.1±11.8 | 53.8±12.2 |
| 磺胺二甲氧嘧啶-D6 Sulfadimethoxine-D6 | 92.2±5.4 | 95.1±6.4 |
| 磺胺嘧啶-D4 Sulfadiazine-D4 | 56.3±8.8 | 52.2±8.9 |
| 甲氧苄啶-13C3 Trimethoprim-13C3 | 102.1±7.1 | 95.7±7.1 |
| NP-AOZ-D4 | 85.5±7.5 | 77.1±7.9 |
| NP-AMOZ-D5 | 71.5±9.1 | 76.1±7.5 |
| NP-AHD-13C3 | 83.3±12.4 | 78.0±8.8 |
| 氯霉素-D5 Chloramphenicol-D5 | 33.6±10.7 | 38.2±14.4 |
| 环丙沙星-D8 Ciprofloxacin-D8 | 109.6±8.2 | 102.6±7.9 |
| 诺氟沙星-D4 Norfloxacin-D4 | 110.4±7.1 | 104.7±6.3 |
1.6 数据分析
采用统计分析软件IBM-SPSS Statistics 22对闽江不同区域(闽江河口上游、北港、南港和下游)抗生素含量的差异进行单因素方差分析(One-way ANOVA),并采用Tukey’s检验差异的显著性。采用独立样本T-检验分析闽江表层水中抗生素总含量的季节性差异。
2 结果与分析
2.1 闽江抗生素类污染物的组成及特征
2.1.1 闽江抗生素类污染物的组成
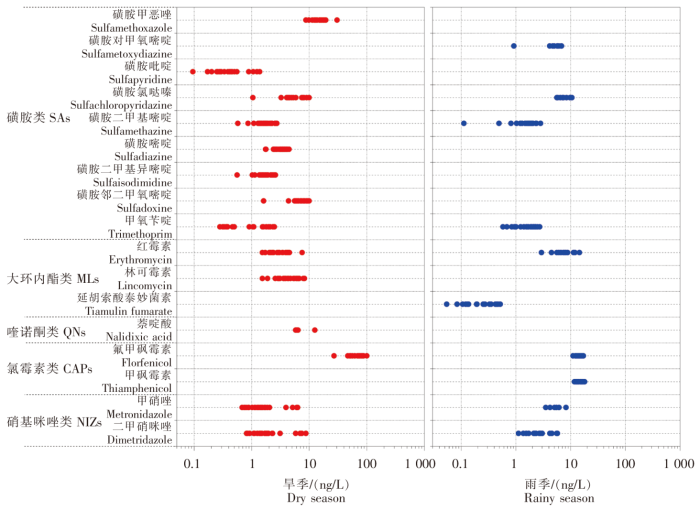
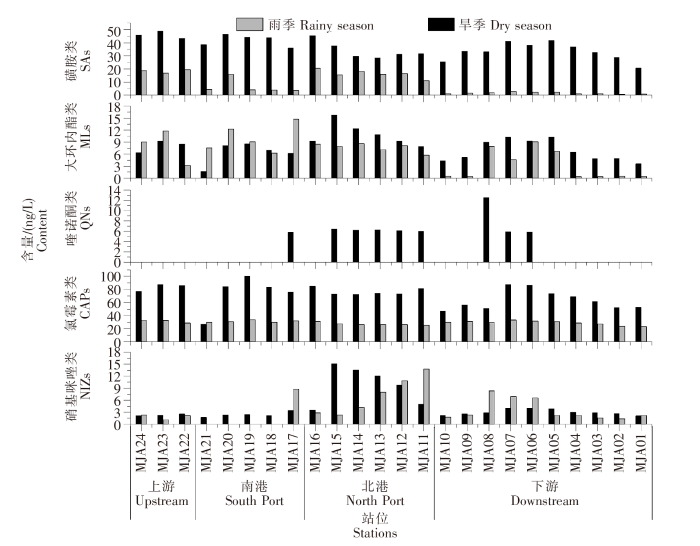
对旱季和雨季采集于闽江24个站位(图1)的表层水样品中的9类88种目标抗生素分别进行了考察,结果共检出5大类17种抗生素(图2),检出总量范围为26.31~155.39 ng/L。在旱季,抗生素总量变化范围在69.22~155.39 ng/L,平均值为123.47 ng/L,标准偏差为24.95 ng/L,共检出14种,分别为磺胺类8种、大环内酯类2种、喹诺酮类1种、氯霉素类1种、硝基咪唑类2种;而在雨季,抗生素总量范围为26.31~69.95 ng/L,平均值为47.61 ng/L,标准偏差为12.07 ng/L,检出10种,分别为磺胺类4种、大环内酯类2种、氯霉素类2种、硝基咪唑类2种。磺胺类、喹诺酮类和大环内酯类污染物含量水平与2017年李文最等[21]在闽江河口上游调查结果处于同一量级,且四环素和β-内酰胺均未检出,但在本研究中发现氯霉素类是闽江河口水体抗生素类污染物的主要组分。与不同流域抗生素污染情况比较,闽江河口区水体中抗生素污染处于相对较低水平,远低于海河、珠江(中国)及昆士兰(澳大利亚),与长江(南京段)及九龙江含量水平相当,但远高于澜沧江(表1)。
图2
图2
旱季和雨季闽江河口区抗生素类污染物检出情况
Fig.2
Detection of antibiotic pollutants in dry and rainy seasons in Minjiang River Estuary
表1 国内外不同流域抗生素污染情况
Tab.1
| 研究区域 Study area | 调查时间 Survey time | 检出种类n,[浓度/(ng/L)] Detected number,concentration | ||||
|---|---|---|---|---|---|---|
| 磺胺类 SAs | 喹诺酮类 QNs | 大环内酯 MLs | 四环素类 TCs | 氯霉素 CAPs | ||
| 闽江-福州段(本研究) Minjiang River-Fuzhou section(this study) | 2018—2019 | 8 (旱季20.69~49.04) (雨季0.58~20.48) | 1 (旱季ND~12.53) (雨季 ND) | 3 (旱季1.72~15.80) (雨季0.33~14.71) | - | 2 (旱季27.00~100.09) (雨季23.42~33.37) |
| 长江(南京段)[22] Yangtze River- Nanjing section | 2018 | 4 (16.27) | 3 (2.26) | 5 (68.17) | 1 (6.25) | 1 (0.51) |
| 珠江(广州段)[18] Pearl River- Guangzhou section | 2015—2016 | 8 (旱季159.72) (雨季268.30) | 3 (旱季111.08) (雨季83.78) | 4 (旱季317.60) (雨季153.11) | 1 (旱季29.30) (雨季35.80) | - |
| 海河[17] Haihe River | 2018 | 5 (496.4) | 1 (21.2) | 3 (62.8) | 3 (16 277) | - |
| 九龙江[15] Jiulong River | 2018 | 7 (0.10~1 205.6) | 6 (ND~43.5) | 4 (1.7~732.4) | - | 3 (0.4~363.6) |
| 九龙江[23] Jiulong River | 2009 | 9 (ND~122.7) | 6 (ND~26.4) | - | 4 (ND~16.9) | 3 (ND~26.4) |
| 澜沧江[24] Lancang River | 2017—2018 | 12 (1.5~23.56) | 5 (0.03~1.45) | 9 (1.03~8.95) | 11 (ND~12.19) | - |
| 多瑙河(罗马尼亚段)[25] Danube River- Romanian section | 2014 | 2 (ND~30) | - | 2 (ND~39) | - | 1 (ND~13) |
| 东南昆士兰(澳大利亚)[26] South East Queensland (Australia) | 2005—2006 | 4 (ND~2 000) | 4 (ND~1 300) | 7 (ND~350) | 4 (ND~600) | - |
注:“-”表示该数据未获得。
Note:- indicated the data was not obtained.
2.1.2 闽江抗生素类污染物的季节差异
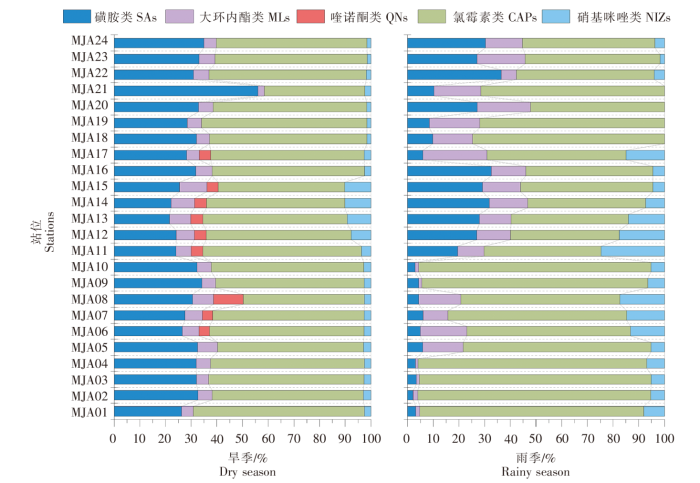
图3
图3
旱季和雨季闽江河口区各类抗生素含量占比
Fig.3
Proportion of various antibiotics in dry season and rainy season in Minjiang River Estuary
磺胺类在旱季和雨季的平均含量分别为36.89 ng/L和8.33 ng/L,相差约3倍,且种类不同。在旱季,磺胺甲恶唑占比为43%,而在雨季,磺胺氯哒嗪占比为39%,磺胺甲恶唑则未检出。水环境中的磺胺类污染物具有高度稳定性,对水生生物特别是胚胎及幼体具有明显的毒性,并可能对其发育造成影响[28]。考察的17种喹诺酮类抗生素中仅萘啶酸在旱季有检出,平均含量为2.55 ng/L,检出率为38.0%。大环内酯在旱季和雨季的平均含量分别为7.89 ng/L和6.27 ng/L,含量水平相差不大但组成不同,旱季为红霉素(43%)和林可霉素(57%),雨季为红霉素(95%)和延胡索酸泰妙菌素(5%)。延胡索酸泰妙菌素可用于治疗家禽类慢性呼吸道病、家畜支原体肺炎,这两种大环内脂类抗生素在畜牧养殖中应用广泛[29]。氯霉素类在旱季只检出氟甲砜霉素1种,平均含量为71.65 ng/L;在雨季检出2种,为氟甲砜霉素和甲砜霉素(各50%),平均含量为29.20 ng/L。氯霉素在农业生产中可以有效治疗畜禽类致病革兰氏阴性菌疾病,但其在环境中极稳定,具有致癌风险[30]。我国在2019年将氯霉素列入食品动物中禁止使用的药品,但近年来氯霉素类抗生素仍在环境[31]及水产品[32]中被检出。氯霉素是闽江河口区水体中占比最高的抗生素类污染物,在雨季和旱季所有站位均有检出,表明其可能仍存在被大量使用的情况,应当引起足够重视。硝基咪唑类在旱季和雨季均检出2种,为甲硝唑和二甲硝咪唑,两季含量水平与组分占比均相近。世界卫生组织(WHO)在2017年将甲硝唑列为2B类致癌物,进入河口环境中的甲硝唑污染物极易溶于水,不易降解,在沉积物中的累积作用显著[33-34]。雨季和旱季不同类别抗生素在检出种类和含量水平上表现出较大的差异,其影响因素有很多种,一方面雨季径流量较大对污染物可能产生较强的稀释作用,另一方面本研究中检出的抗生素多用于养殖行业,不同季节养殖过程中抗生素的用量也有较大区别[35-36]。此外,抗生素的光降解和生物降解在不同季节也有着较大的差异[37]。
2.1.3 闽江抗生素类污染物含量的时空变化特征
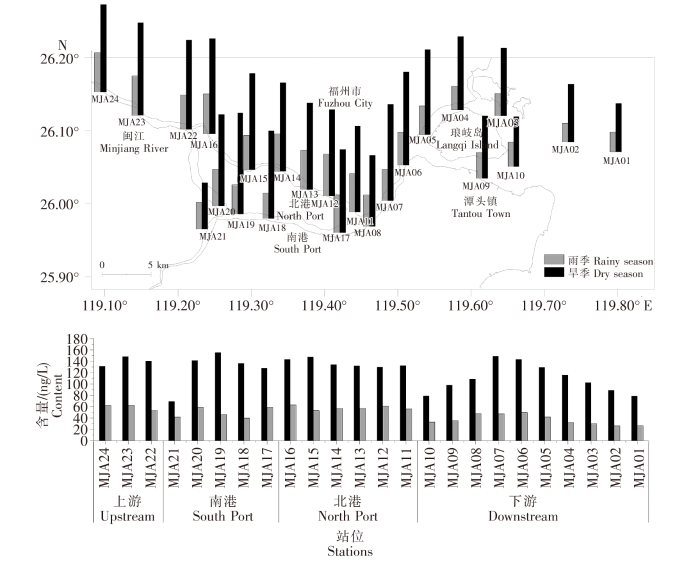
图4
图4
闽江河口区水体抗生素类污染物含量的时空分布
Fig.4
Temporal and spatial distribution of antibiotic pollutants in Minjiang River Estuary waters
表2 闽江不同区域表层水中各类抗生素含量
Tab.2
| 季节 Season | 区域 Area | 磺胺类 SAs | 大环内酯类 MLs | 喹诺酮类 QNs | 氯霉素类 CAPs | 硝基咪唑类 NIZs | 总量 Total content |
|---|---|---|---|---|---|---|---|
| 旱季 Dry season | 上游 | 46.15±2.81a | 8.04±1.50a | ND | 83.55±5.79a | 2.3±0.25a | 140.05±8.47a |
| 北港 | 34.07±6.46b | 10.9±2.84a | 5.17±2.54a | 76.53±5.39a | 9.85±4.68b | 136.51±7.23a | |
| 南港 | 41.86±4.28ab | 6.32±2.73a | 1.16±2.60a | 74.27±27.82a | 2.42±0.65a | 126.03±33.30a | |
| 下游 | 33.31±6.75b | 6.82±2.59a | 2.43±4.31a | 63.83±14.76a | 3.00±0.70a | 109.40±25.00a | |
| 雨季 Rainy season | 上游 | 18.45±1.43a | 7.98±4.38ab | ND | 31.27±2.11a | 1.84±0.63a | 59.54±4.99a |
| 北港 | 16.24±3.19a | 7.66±1.09ab | ND | 27.05±2.12a | 6.99±4.68a | 57.94±3.60a | |
| 南港 | 6.28±5.35b | 9.98±3.46b | ND | 31.09±1.52a | 1.76±3.93a | 49.11±9.10ab | |
| 下游 | 1.56±0.81b | 3.07±3.61a | ND | 28.92±3.18a | 3.53±2.64a | 37.09±8.93b |
注:1.以字母的不同来表示差异的显著;2.ND表示未检出。
Note:1.Different letters were used to indicate the significant difference;2.ND indicated not detected.
闽江河口区各类抗生素类污染物含量的时空分布如表2和图5所示。在旱季,磺胺类呈现出上游显著高于北港和下游地区(P<0.05),在雨季则呈现出上游和北港显著高于南港和下游(P<0.05),由此可见,闽江河口区域的磺胺类抗生素可能主要来源于上游的输入。喹诺酮类仅在旱季有检出,且检出的站位主要分布在北港以及南北港交汇处,这可能意味着福州的城市输入是闽江喹诺酮类抗生素的主要来源。大环内酯类仅在雨季表现出南港显著高于下游,而硝基咪唑类仅在旱季表现出北港显著高于上游、南港和下游(P<0.05),这可能是由于在不同季节,这两类抗生素输入源有所不同,在雨季,雨水的冲刷可能会使南港区域大环内酯类药物大量进入闽江南港区域,使其含量显著高于下游地区;在旱季,北港区域硝基咪唑类抗生素的显著提高可能是由于旱季闽江径流量减少,闽江北港区域含有硝基咪唑类抗生素的生活污水排放所致。氯霉素类抗生素因其性质稳定,在旱季和雨季不同区域间抗生素含量差异均不显著,这说明该类污染物可在河口区域稳定存在。
图5
图5
闽江河口区各类抗生素类污染物含量的时空分布
Fig.5
Temporal and spatial distribution of antibiotic pollutants in Minjiang River Estuary
2.2 闽江抗生素类污染物的风险评价
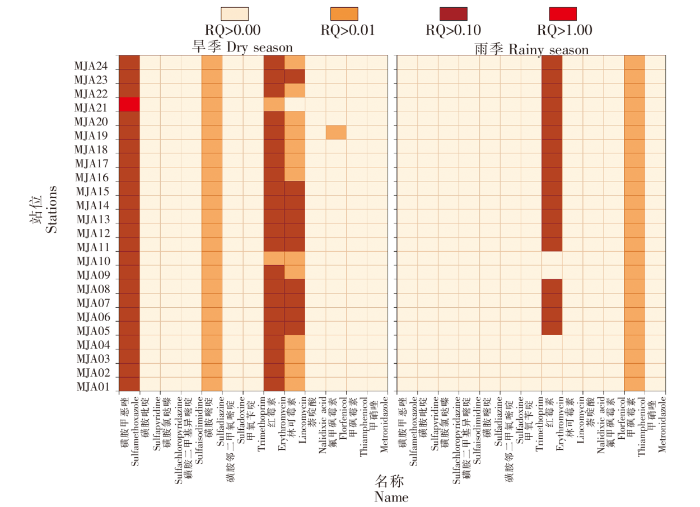
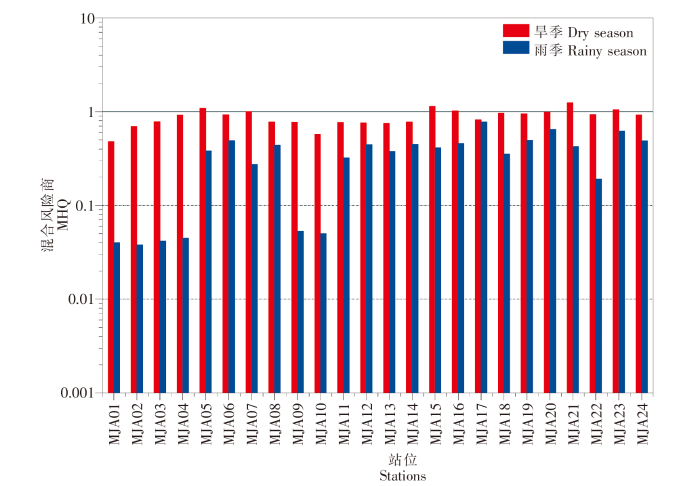
闽江水体中抗生素类污染物的风险评价结果以及联合风险商见图6和图7。从图6中可以看出,在旱季,磺胺甲恶唑的RQ值在MJA21站位大于1.0,为高生态风险,其余站位均处于中等生态风险;红霉素(92%站位)和林可霉素(42%站位)RQ值在0.1~1.0范围,具有中等生态风险;在雨季,红霉素(75%站位)RQ值在0.1~1.0范围,为中等生态风险。从MHQ计算结果来看,在旱季,尽管只有25%的站位MHQ大于1.0,显示出高生态风险,但24个站位平均MHQ值为0.88,接近于高风险阈值。此外,雨季除河口下游部分站位显示为低生态风险外,河口上游、北港和南港均显示为中等生态风险,值得进一步关注并采取有效控制措施。由于磺胺对甲氧嘧啶、磺胺二甲基异嘧啶、延胡索酸泰妙菌素、二甲硝咪唑、克球酚、金刚烷胺的相关独立数据缺乏,导致其在环境中的PNEC值无法获得,RQ值无法计算,因此可能会低估闽江抗生素类污染物的生态风险。
图6
图6
不同季节闽江河口区抗生素类污染物RQ值
Fig.6
RQ values of antibiotic pollutants in Minjiang River Estuary in different seasons
图7
图7
闽江河口区各站位不同季节MHQ值
Fig.7
MHQ in different seasons at each station in Minjiang River Estuary
3 结论
在本研究中,闽江河口区水体在旱季和雨季共检测到5类17种抗生素类污染物,总含量变化范围在26.31~155.39 ng/L,与国内外其他流域相比,闽江河口水体中抗生素含量处于相对较低的水平。从空间分布来看,在闽江河口上游、北港和南港抗生素总量变化不大,河口下游受海水稀释作用影响而抗生素含量呈明显下降的趋势。不同种类抗生素在不同季节具有相对不同的空间分布特征,其中喹诺酮类和硝基咪唑类在人口密集的北港区域污染较严重。在旱季,磺胺甲恶唑具有高生态风险,红霉素和林可霉素具有中等生态风险;在雨季,红霉素显示中等生态风险。从MHQ计算结果来看,闽江河口区大部分站位均处于高生态风险阈值左右,值得相关管理部门进一步关注并制定有效管控措施。
参考文献
Antibiotics in the aquatic environment - A review - Part Ⅰ
[J].
Antibiotics in soil and water in China-a systematic review and source analysis
[J].
Distribution,abundance,and risk assessment of selected antibiotics in a shallow freshwater body used for drinking water,China
[J].
Occurrence and distribution of antibiotics in sediments from black-odor ditches in urban areas from China
[J].
Antibiotics and antibiotic resistant genes(ARGs)in groundwater:a global review on dissemination,sources,interactions,environmental and human health risks
[J].
Swine farming elevated the proliferation of Acinetobacter with the prevalence of antibiotic resistance genes in the groundwater
[J].
Biofilms as a sink for antibiotic resistance genes(ARGs)in the Yangtze Estuary
[J].
The distribution and partitioning of common antibiotics in water and sediment of the Pearl River Estuary,South China
[J].
Occurrences of three classes of antibiotics in a natural river basin:association with antibiotic-resistant Escherichia coli
[J].
闽江口水环境主要理化因子时空分布特征研究
[J].对闽江口海域春秋两季的水质进行调查,应用主成分分析法(PCA)进行统计,以研究水质状况、10个水质理化因子的时空分布特征以及闽江径流陆源入海污染物情况。结果表明:1)无机氮(DIN)全部超标,化学需氧量(COD)和活性磷酸盐(PO43--P)存在不同程度超标,但多年数据显示DIN污染情况逐渐好转;2)COD、DIN等在空间上呈现出以琅岐岛为中心向外海逐渐递减,PO43--P分布特征相反,时间上表现为春季水质略差于秋季的分布特征;3)溶解氧(DO)、亚硝酸盐(NO2--N)、铵盐(NH4+-N)和PO43--P是海域水质污染的主要驱动因子,其中,悬浮物(SS)、硝酸盐(NO3--N)、NO2--N、NH4+-N主要来自闽江径流输入,并成为闽江口海域主要污染源。
闽江口潮间带大型底栖动物群落基本特征分析
[J].2013年至2019年在闽江口进行了11个航次共38个断面的潮间带大型底栖动物调查研究,共发现潮间带生物195种,隶属10个门类,主要以甲壳类、软体动物和多毛类为主。敖江入海口潮间带生物的物种多样性、生物量和丰度均显著高于闽江入海口,且敖江入海口潮间带生物的多样性指数(H′)、均匀度指数(J′)和丰富度指数(D)也均显著高于闽江入海口。闽江口潮间带生物的物种数、丰度和生物量在中、低潮区均显著高于高潮区。闽江入海口潮间带的优势种以小型蟹类为主,敖江入海口潮间带的优势种包括多毛类、软体动物和蟹类,其中经济种类菲律宾蛤仔(Ruditapes philippinarum)和焦河蓝蛤(Potamocorbula ustulata)为敖江入海口的主要优势种。敖江入海口的潮间带生物需要更多的关注和研究。
Characterization of antibiotics in a large-scale river system of China:occurrence pattern,spatiotemporal distribution and environmental risks
[J].
Predictive environmental risk assessment of chemical mixtures:a conceptual framework
[J].Environmental risks of chemicals are still often assessed substance-by-substance, neglecting mixture effects. This may result in risk underestimations, as the typical exposure is toward multicomponent chemical "cocktails". We use the two well established mixture toxicity concepts (Concentration Addition (CA) and Independent Action (IA)) for providing a tiered outline for environmental hazard and risk assessments of mixtures, focusing on general industrial chemicals and assuming that the "base set" of data (EC50s for algae, crustaceans, fish) is available. As mixture toxicities higher than predicted by CA are rare findings, we suggest applying CA as a precautious first tier, irrespective of the modes/mechanisms of action of the mixture components. In particular, we prove that summing up PEC/PNEC ratios might serve as a justifiable CA-approximation, in order to estimate in a first tier assessment whether there is a potential risk for an exposed ecosystem if only base-set data are available. This makes optimum use of existing single substance assessments as more demanding mixture investigations are requested only if there are first indications of an environmental risk. Finally we suggest to call for mode-of-action driven analyses only if error estimations indicate the possibility for substantial differences between CA- and IA-based assessments.
Occurrence and risk assessment of antibiotics in surface water and groundwater from different depths of aquifers:a case study at Jianghan Plain,central China
[J].
Antibiotics pollution in Jiulong River Estuary:source,distribution and bacterial resistance
[J].
High sensitive multiresidue analysis of pharmaceuticals and antifungals in surface water using U-HPLC-Q-Exactive Orbitrap HRMS.Application to the Danube River basin on the Romanian territory
[J].
The occurrence of antibiotics in an urban watershed:from wastewater to drinking water
[J].The presence of 28 antibiotics in three hospital effluents, five wastewater treatment plants (WWTPs), six rivers and a drinking water storage catchment were investigated within watersheds of South-East Queensland, Australia. All antibiotics were detected at least once, with the exception of the polypeptide bacitracin which was not detected at all. Antibiotics were found in hospital effluent ranging from 0.01-14.5 microg L(-1), dominated by the beta-lactam, quinolone and sulphonamide groups. Antibiotics were found in WWTP influent up to 64 microg L(-1), dominated by the beta-lactam, quinolone and sulphonamide groups. Investigated WWTPs were highly effective in removing antibiotics from the water phase, with an average removal rate of greater than 80% for all targeted antibiotics. However, antibiotics were still detected in WWTP effluents in the low ng L(-1) range up to a maximum of 3.4 microg L(-1), with the macrolide, quinolone and sulphonamide antibiotics most prevalent. Similarly, antibiotics were detected quite frequently in the low ng L(-1) range, up to 2 microg L(-1) in the surface waters of six investigated rivers including freshwater, estuarine and marine samples. The total investigated antibiotic concentration (TIAC) within the Nerang River was significantly lower (p<0.05) than all other rivers sampled. The absence of WWTP discharge to this river is a likely explanation for the significantly lower TIAC and suggests that WWTP discharges are a dominant source of antibiotics to investigated surface waters. A significant difference (p<0.001) was identified between TIACs at surface water sites with WWTP discharge compared to sites with no WWTP discharge, providing further evidence that WWTPs are an important source of antibiotics to streams. Despite the presence of antibiotics in surface waters used for drinking water extraction, no targeted antibiotics were detected in any drinking water samples.
Thermal degradation of chloramphenicol in model solutions,spiked tissues and incurred samples
[J].This study investigated the thermal degradation of a veterinary drug, chloramphenicol, in model solutions (water), as well as in spiked and incurred mussel tissues to understand its fate in the food supply chain. Thermal degradation kinetics followed a first-order model in water (e.g. degradation rate: 0.0018-0.0025 min at 100 °C). After 1 h at 100 °C, the percentage degradation in spiked tissues (28.1 ± 7.1%) was significantly different (p < .05) from the values in water (14.2 ± 1.6%) and incurred mussel tissues (19.0 ± 4.1%). Using liquid chromatography coupled to high-resolution accurate mass tandem mass spectrometry, the resulting degradation products of chloramphenicol were identified in water, spiked and incurred tissues, and were all different. Therefore, although the use of water models and spiking food samples may provide some information, our data confirm that "incurred models" should be systematically implemented to provide reliable information about veterinary drug residue stability for food safety risk assessments.Copyright © 2017 Elsevier Ltd. All rights reserved.
Determination of metronidazole residues in water,sediment and fish tissue samples
[J].Metronidazole (MNZ) is an antibacterial and antiprotozoal drug used in veterinary and human medicine. Its continual entry into the environment and its biological properties may have significant, long-term effects on the stability of ecosystems because MNZ and its metabolites possess mutagenic, carcinogenic and toxic properties. For this reason, the application of MNZ in food-producing species is prohibited in the EU, the USA and other countries. To ensure human food safety and to protect the environment, robust and reliable screening and confirmatory tests capable of the low-level detection of MNZ residues are required. The development of methods for MNZ determination in biological and environmental samples is thus an important analytical task in environmental and food science. This work focuses on the evaluation of a method for determining MNZ in water, sediment and fish tissue samples using liquid chromatography - ion trap mass spectrometry (LC-MS/MS). MNZ was extracted from waters on Strata XC cartridges using solid phase extraction (SPE), and from sediments and fish tissues by solid-liquid extraction (sediment: 15 mL 0.1 M HCl (pH = 0.6), 15 min; fish tissue: 15 mL 1% CH3COOH in ACN, 1 min; drying: 5 g MgSO4((anhyd).; 30 s) with SPE purification of the extracts (from sediment: Strata XC cartridge; from fish tissue: Supelco NH2 cartridge). The optimal procedure that we developed was validated in order to confirm its reliability and sensitivity. Matrix effects (ME) were established. Absolute recoveries ranged from 89.3% to 97.2%, and the method detection limits were 3.4 ng L-1 (water samples), 0.4 ng g(-1) (sediment samples) and 0.3 ng g(-1) (tissue samples). These methods were used to determine MNZ in surface waters, sediments and fish tissues from the Polish River Gosicina; MNZ was found in all these matrices. The highest concentrations in water, sediment and tissue were 136.2 ng L-1, 12.0 ng g(-1) and 1.5 ng g(-1) respectively. The results confirmed that these methods are suitable for the simultaneous analysis of waters, sediments and fish tissues for the presence of MNZ. (C) 2014 Elsevier Ltd.
Degradation of metronidazole by radio frequency discharge in an aqueous solution
[J].
Antibiotics in typical marine aquaculture farms surrounding Hailing Island,South China:occurrence,bioaccumulation and human dietary exposure
[J].